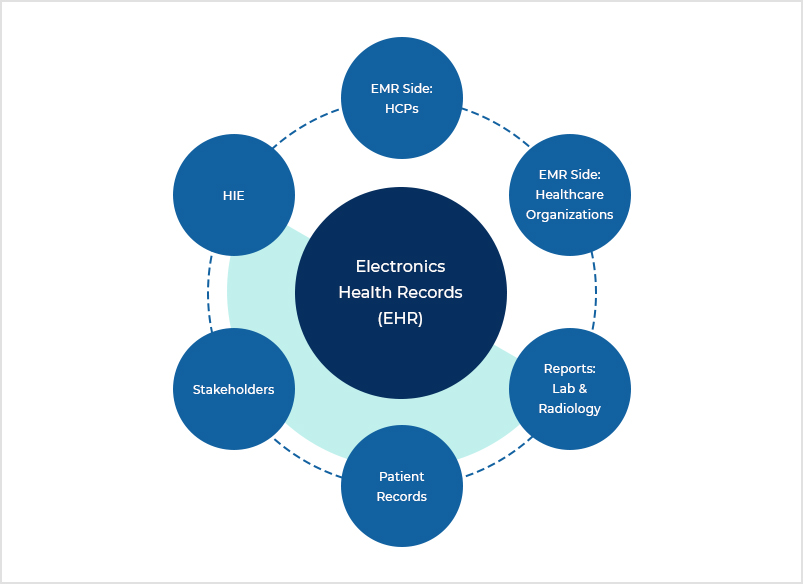
Master Facets hands-on from basic to advanced level concepts with real-time examples. Our training will help you gain in-depth knowledge of claims processing and automating tasks using Facets workflow application through hands-on sessions. By the end of the training, you’ll become an expert in applying this knowledge in real-world. Master Facets hands-on from basic to advanced level concepts with real-time examples. Our training will help you gain in-depth knowledge of claims processing and automating tasks using Facets workflow application through hands-on sessions. By the end of the training, you’ll become an expert in applying this knowledge in real-world. The Facets Core Administration platform, trusted by more than 75 healthcare organizations, consists of a rich set of modules that allow payer organizations to meet their business requirements while positioning them for growth and change. Healthcare FACETS System Facets (Trizetto Claims processing system) provides several functionality which is supported under the application group or you can call modules.It helps the organizations to perform their day to day operational work by utilizing any or all of the application groups.

Facets Healthcare Tables
Facets Healthcare Claims
Agile Health Technologies Inc. is a healthcare information technology company offering specialized business and technology solutions and services in product areas such as FACETS and QNXT for our Health Plan clients.
FACETS, one of the flagship products of Trizetto, is an excellent Health Plan core administration solution. However, like any enterprise product, from implementation to operation and production support, it requires configurations, customizations, extensions and interfaces to meet the client-specific business requirements. With constant changes in business rules, government mandates, technological advances etc., there is a constant need to upgrade and changes to the enterprise application without impacting the core systems.
FACETS Healthcare – At Agile, our highly skilled FACETS experts are helping our clients in utilizing the fullest potential of the FACETS system through seamless integration, configuration, extensions, upgrades and testing through our blended-shore FACETS Center of Excellence. Whether it is Plan / Product configuration, Provider Networks or Fee Schedule, NetworX Pricing, ExternalClaims and Accumulator updates, Workflow management integrating external applications like Claims Xtend; our
Center of Excellence is the best and most cost-effective alternative to OEM resources. We are your partner in your healthcare business operation using FACETS.

FACETS Healthcare Technology, We located in Naperville, IL and Bangalore, India; provides the perfect mix of onshore – offsite team composition managed through our robust RMO and project delivery which is managed by the PMO process. This “follow the sun”
model of delivery brings in –
• Reduces implementation and operational cost for our clients
• Enables 24-hour support
• Faster delivery
• High quality due to both onshore and offsite quality inspections
• Ability to expand and contract staffing based on current needs

We are a Hi-TRUST accessed and Hi-Tech Associates security certified and HIPAA compliant organization.
The agile healthcare technology company, our Center of Excellence is providing best in class Outsourcing services in the following areas –
• Provider and Network Management – We at Agile help our Clients manage their annual Provider and network assignment along with the agreements. We help set up the agreements and conduct user acceptance testing on their behalf.
• Configuration and Benefits Management – Every year Health Plans roll out new products and changes. We help our Clients in configuration and benefits validation using our proprietary benefit testing Tool BenefitPro or Client specific tools.
• Pricing and Agreements – We specialize in Managing provider pricing and Network configuration. We configure agreements and pricing and validate the pricing using custom reports and Claim Processing.
• Enrolment and Billing – Our Services include Validation of new enrolment process and systems, annual rate validation and specimen billing validation. Billing reconciliation and Broker Commission processing
• Claims Analytics and Recovery – We assist Clients in their analytics by providing ad hoc reporting and data presentation. We also help in their overpayment recovery process and corrections. We also perform validation for Configuration changes, Productions Incidents and new changes.
Our Outsourcing model employs a flexible resource plan, duration and schedule based on clients need. Our model offers the unique blend of Knowledge and flexibility which can assist Clients in their operation and increase savings.
